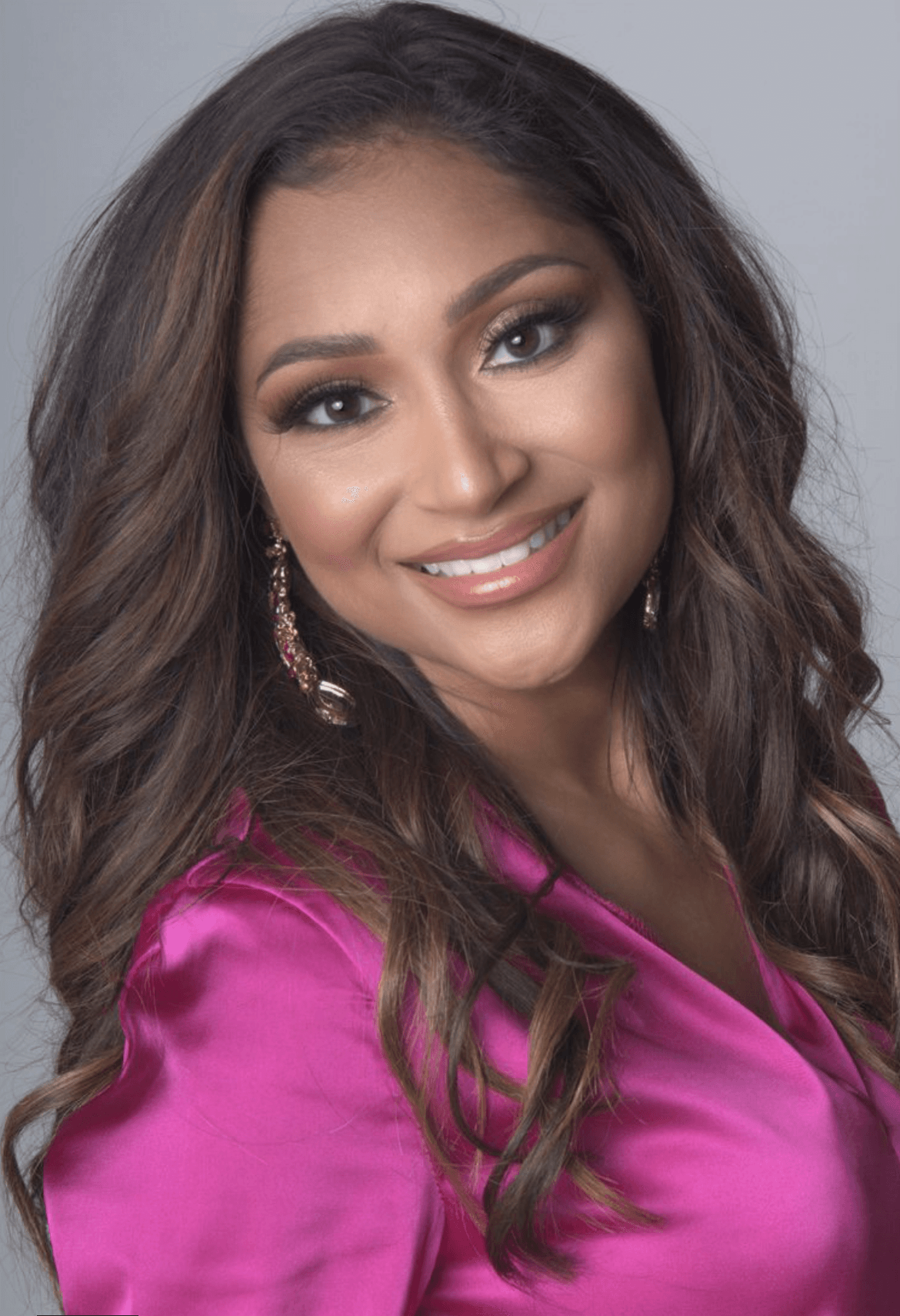
We’re excited to introduce you to the always interesting and insightful Shoshana Hallowell. We hope you’ll enjoy our conversation with Shoshana below.
Shoshana, looking forward to hearing all of your stories today. Let’s kick things off with talking about how you serve the underserved, because in our view this is one of the most important things the small business community does for society – by serving those who the giant corporations ignore, small business helps create a more inclusive and just world for all of us.
Operation Breast Density is a 501(c)(3) nonprofit organization dedicated to improving breast cancer detection and survival through education, advocacy, and access to care. The organization raises awareness about the critical impact of breast density—a factor that not only increases a woman’s risk of developing breast cancer but also makes it more difficult to detect cancer on mammograms.
Operation Breast Density educates both clinicians and the public about the importance of individualized breast cancer screening based on personal risk factors, including breast density, rather than relying on outdated, one-size-fits-all guidelines.
In addition to its educational outreach, the nonprofit provides financial assistance for supplemental imaging such as breast ultrasound or MRI to women who have dense breast tissue but lack insurance coverage or the resources to afford these potentially life-saving tests. Through partnerships with imaging centers and ongoing community fundraising events, Operation Breast Density strives to ensure that all women—regardless of income—have access to the advanced screening they need to detect breast cancer early.

Shoshana, before we move on to more of these sorts of questions, can you take some time to bring our readers up to speed on you and what you do?
Cancer has always been a part of my life. Every day as a General Surgeon, I confront its presence while treating patients battling this disease. Some days, I deliver the relieving news of remission, while on others, I must convey the unwelcome recurrence. However, my relationship with cancer took on a profoundly personal dimension when, at the age of 37, I received my own diagnosis.
Despite being deeply entrenched in the demands of my profession, I neglected to address a lump in my breast for several months, prioritizing patient care over self-care. Upon finally undergoing imaging and reviewing the results, the realization struck me like a bolt of lightning—I had committed the very mistake I caution my patients against: delaying my own medical attention.
Within days of the imaging, I underwent a biopsy and, amidst the whirlwind of my hectic schedule, received a call that forever altered the trajectory of my life: “Dr. Hallowell, the biopsy results are positive for cancer.”
As a surgeon intimately acquainted with the options, I opted for the most aggressive approach—undergoing a bilateral mastectomy with delayed reconstruction over the course of 2020-2021. While my journey towards recovery is still fraught with challenges, including a five-year regimen of anti-hormone therapy, I’m grateful to have avoided some of the more arduous treatment paths endured by many others in similar circumstances.
Following my diagnosis, I urged my sisters and mother to undergo additional screening imaging, given their elevated risk as my first-degree relatives now affected by cancer. Specifically, I emphasized to my sister the importance of informing her primary care physician (PCP) about her heightened risk factors for breast cancer and advocated for her to undergo a Breast MRI for screening.
However, despite my insistence, her PCP advised waiting six months for the imaging, citing a “normal” mammogram. What my sister wasn’t told, however, was that her mammogram had indicated dense breasts. This detail is crucial, as mammograms miss a cancer diagnosis up to 50% of the time in women with dense breast tissue. Therefore, regardless of family history, additional imaging for breast cancer screening was warranted for my sister.
Six months later, my sister finally underwent the Breast MRI, revealing a 2.3 cm triple-negative breast cancer. Immediately, I requested to review my sister’s mammogram reports from previous years, only to discover that they consistently indicated dense breast tissue over the past four years. She should have undergone the MRI four years ago!
Following this discovery, my family and I recognized the urgency for my mother to undergo imaging as well. Despite being 75 years old at the time and having had her last mammogram two years prior, we were alarmed to learn that according to the US Preventative Service Task Force, mammography isn’t routinely recommended for women over 75. However, the American Cancer Society advises continuing screening for elderly women with a life expectancy of more than 10 years.
Given my mother’s vibrant health and active lifestyle, it became evident that she wasn’t receiving appropriate screening from her PCP. The realization left me questioning how this oversight had occurred without my knowledge. Promptly, we scheduled her for a mammogram the following week, and within two weeks, my mother received a diagnosis of DCIS.
I was utterly astonished! As someone deeply entrenched in the medical field and specializing in treating breast cancer, it was shocking to discover that my own family members weren’t receiving appropriate breast cancer screening. How had I not been aware of this oversight? I had assumed their physicians were diligently caring for them, evaluating their risk factors. Unfortunately, this wasn’t the reality, and as a result, both my sister and mother suffered delays in diagnosis.
Reflecting on this experience, I couldn’t help but think about the countless other women who might be facing similar challenges. It’s estimated that approximately 40% of all women have dense breast tissue and require additional imaging for accurate screening. Moreover, with our elderly population living longer and healthier lives, it’s imperative that age not be a barrier to screening, as early detection significantly impacts cancer survival rates.
What’s even more concerning is the lack of awareness surrounding breast density among women. A staggering 95% of women are unaware of their breast density, despite it increasing their risk of breast cancer by 4-6 times. Although this knowledge has existed within the medical community, its dissemination to the public and integration into patient care has been delayed.
Progress has been made, notably with Nancy Capello’s advocacy leading to the implementation of breast density reporting laws, but enforcement remains inconsistent. Furthermore, screening guidelines for women with dense breasts have stagnated since 2015, despite evidence suggesting that modalities such as ultrasound, molecular breast imaging (MBI), and MRI are more effective in detecting cancers in this population.
In response to these glaring gaps in care, I’ve made a personal commitment. I vow not only to advocate for my sister and mother but for all women. It’s imperative that women are informed about their breast density and associated risks, that physicians order appropriate screening modalities, and that insurance companies provide coverage for these vital screenings. Early detection is paramount for ensuring women’s survival, and I’m dedicated to doing whatever it takes to make sure this doesn’t continue to happen.was astonished! Not only am I in the medical field, but I treat breast cancer and my own family members were not being screened appropriately for breast cancer. How did I not know they were not getting the appropriate care? I just assumed their physicians were taking care of them. I assumed their risk factors were being evaluated. This was not the case and due to this my sister and mother suffered a delay in diagnosis. If this is happening to people with medical knowledge and medical advocates that even bring the information to their physician about the additional screening needs and are still denied proper care then can you imaging how many other women are being effected. I can tell you – its about 40% of all women. 40% of women have dense breast tissue and require this additional imaging. In addition, our elderly population is growing and living much longer and healthier lives. By no means should their screening be cut off due to age. Cancer survival depends on the stage at diagnosis therefore screening is essential.
I was utterly astonished! As someone deeply entrenched in the medical field and specializing in treating breast cancer, it was shocking to discover that my own family members weren’t receiving appropriate breast cancer screening. How had I not been aware of this oversight? I had assumed their physicians were diligently caring for them, evaluating their risk factors. Unfortunately, this wasn’t the reality, and as a result, both my sister and mother suffered delays in diagnosis.
Reflecting on this experience, I couldn’t help but think about the countless other women who might be facing similar challenges. It’s estimated that approximately 40% of all women have dense breast tissue and require additional imaging for accurate screening. Moreover, with our elderly population living longer and healthier lives, it’s imperative that age not be a barrier to screening, as early detection significantly impacts cancer survival rates.
What’s even more concerning is the lack of awareness surrounding breast density among women. A staggering 95% of women are unaware of their breast density, despite it increasing their risk of breast cancer by 4-6 times. Although this knowledge has existed within the medical community, its dissemination to the public and integration into patient care has been delayed.
95% of women do not know if they have dense breast tissue or not. In addition, 90% of women are not aware that dense breast tissue increase your risk of breast cancer by 4-6 fold. Although this knowledge was known in the medical community its translation to the public and patient care is still significantly delayed. It was not until 2009 when Nancy Capello championed the first in the nation breast density information law in the state of Connecticut. As of 2019 Federal legislation has made density reporting now standard of care in 50 states. However, this is still not always enforced.
In addition, screening guidelines for women with dense breasts have not been updated by the American Cancer Society, National Comprehensive Cancer Network, US Preventative Service Task Force, American College of Obstetrics & Gynecology, and the Academy of Family Physicians since 2015. Since that time there has been data providing evidence that ultrasound, MBI and MRI find significantly more cancers than mammography alone in women with dense breasts, and are able to diagnose those cancers at an earlier age.
I have made it my promise, not only my sister and mother, but to all women that I will do what it takes to make sure this does not continue to happen to women. Women need to be notified of their density and its associated risk, their physicians need to order the appropriate screening modalities indicated for their breast tissue, insurance companies need to provide coverage for these additional screenings and their cancer diagnoses need to be caught as early as possible to ensure their survival. This is why I founded the 501c3 nonprofit organization, Operation Breast Density. This initiative is wholly committed to raising awareness about breast density. Our mission encompasses educating patients, healthcare providers, and physicians about the vital importance of appropriate screening modalities for individuals with dense breast tissue.
Furthermore, Operation Breast Density will tirelessly advocate for the update of screening guidelines by national cancer organizations, ensuring that they reflect the unique needs of this patient population. We’ll also work towards implementing standardized breast cancer risk assessment tools that accurately incorporate breast density, addressing a critical gap in our current models.
Moreover, recognizing the financial barriers that many individuals face, our organization will provide essential support by offering financial assistance to those in need of supplemental screening due to dense breast tissue or other high-risk factors. Together, through education, advocacy, and practical assistance, Operation Breast Density aims to make a tangible difference in the lives of countless individuals affected by breast cancer.
We’d love to hear a story of resilience from your journey.
In 2022, I founded Operation Breast Density, a nonprofit dedicated to educating both clinicians and the community about the impact of breast density and advocating for personalized screening. Most importantly, we provide financial assistance to help women access the additional imaging they need—imaging that is often not covered by insurance despite being medically necessary.
This journey has extended far beyond my own story. My sister—who had a normal mammogram—was later diagnosed with triple-negative breast cancer after I insisted on further imaging due to her breast density. My mother, at 75, was diagnosed with DCIS because I challenged the idea that older women don’t need screening. These were cancers that might have gone undetected without someone to push for more.
What I’ve learned is this: Resilience isn’t just about bouncing back—it’s about rising up and turning pain into purpose. Operation Breast Density was born from that purpose. It’s my way of fighting for every woman to be seen, informed, and screened properly—regardless of income, age, or what’s covered by her insurance.
My story isn’t unique—but that’s exactly why I share it. Because breast cancer doesn’t discriminate, and awareness shouldn’t either.
If you want to be part of this mission, I invite you to learn more at www.operationbreastdensity.org. Let’s save lives—together.

Any advice for managing a team?
Managing a team—especially in a nonprofit setting—requires leading with purpose, clarity, and empathy. For me, it starts with making sure everyone understands and feels connected to our mission. When people know their work is truly making a difference—like helping women access life-saving breast cancer screenings—they’re naturally more engaged and motivated.
I also believe in empowering team members by recognizing their individual strengths, giving them ownership of their roles, and encouraging collaboration. Whether it’s a volunteer, a board member, or a staff lead, I want everyone to feel like their voice matters.
To maintain morale, I try to celebrate the wins—big or small—and always express gratitude. In nonprofit work, where the emotional toll can be heavy and the hours long, a simple “thank you” goes a long way. I’ve learned that creating a culture where people feel seen, supported, and inspired makes all the difference in building a strong, resilient team.
Lastly, I lead by example. As someone who’s walked the road of a breast cancer patient myself, I never forget how personal this work is. That authenticity resonates with my team and keeps us all grounded in why we do what we do.
Contact Info:
- Website: https://www.operationbreastdensity.org
- Instagram: https://www.instagram.com/operationbreastdensity
- Facebook: https://www.facebook.com/operationbreastdensity
- Linkedin: https://www.linkedin.com/operationbreastdensity





