We were lucky to catch up with Karen Wonders recently and have shared our conversation below.
Karen, thanks for joining us, excited to have you contributing your stories and insights. Can you share a story with us from back when you were an intern or apprentice? Maybe it’s a story that illustrates an important lesson you learned or maybe it’s a just a story that makes you laugh (or cry)?
When I was a graduate student intern at a cancer rehabilitation center, I met a patient who completely transformed my perspective on resilience and parenting. Sarah was a young mother in her early thirties who had recently been diagnosed with stage II breast cancer. What made her unique among our patients was that she regularly brought her 9-year-old daughter, Emma, to her exercise sessions.
Initially, I was apprehensive about working with Sarah while Emma watched. I worried that seeing her mother in a clinical setting—attached to a heart rate monitor, sometimes struggling to complete exercises, occasionally needing to rest—would frighten the young girl. I even gently suggested to Sarah that perhaps we could schedule sessions during Emma’s school hours.
Sarah’s response changed everything. “I want her to see this,” she told me firmly. “I want her to see me fight. I want her to know that when life knocks you down, you get back up—even when it’s hard, even when you’re scared.”
Over the next several months, I witnessed something remarkable unfold. Sarah approached each session with unwavering determination. There were days when the fatigue from her treatments was overwhelming, yet she would still complete her modified routine, often looking over at Emma with a smile or a thumbs-up.
What struck me most was their ritual at the end of each session. Emma would hand her mother a water bottle and say, “Good job, Mom. You’re getting stronger.” Sarah would respond, “We both are, sweetheart.”
I realized that what I had initially interpreted as potentially traumatic for Emma was actually an invaluable life lesson. Sarah wasn’t just fighting cancer; she was deliberately modeling courage, perseverance, and hope for her daughter. She wanted Emma to witness firsthand that difficult circumstances don’t define you—your response to them does.
By the end of Sarah’s program, her physical measurements had improved significantly, but the most profound change was in my understanding of what it means to parent through crisis. Sarah taught me that sheltering children from hardship isn’t always the answer; sometimes letting them witness your struggle—and your determination to overcome it—is the greatest gift you can give them.
This experience fundamentally shaped how I approach my work with cancer patients and how I mentor students in exercise oncology. I teach them that our role isn’t just to improve physical function but to honor and support the whole person—including their identities as parents, partners, and role models. Sarah and Emma showed me that rehabilitation can be as much about healing family relationships and building emotional resilience as it is about rebuilding physical strength.

As always, we appreciate you sharing your insights and we’ve got a few more questions for you, but before we get to all of that can you take a minute to introduce yourself and give our readers some of your back background and context?
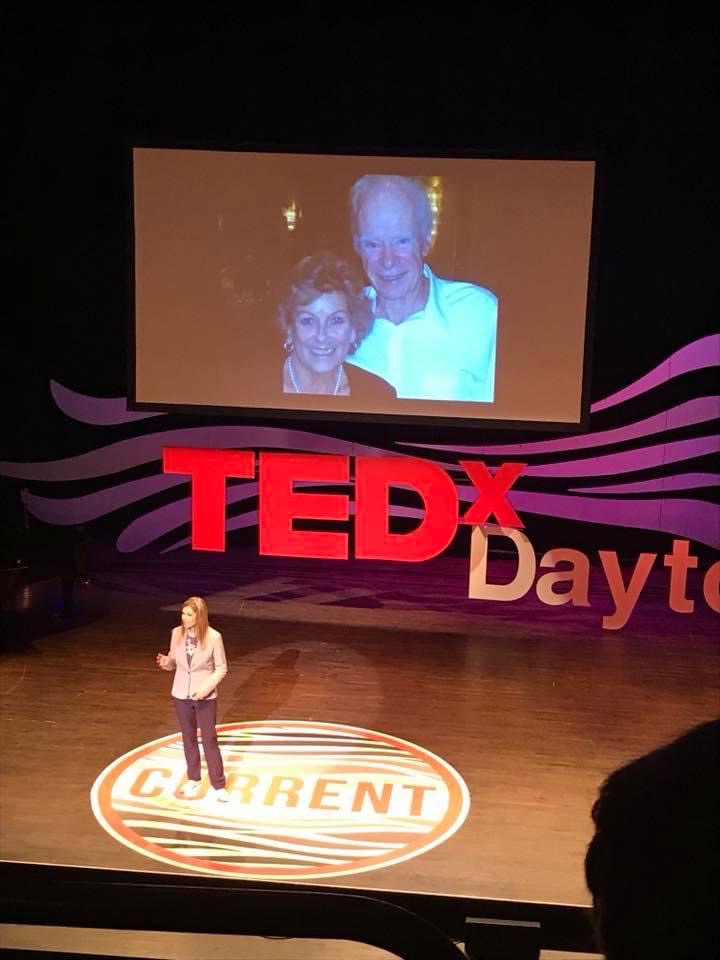
I’m Dr. Karen Wonders, a Professor and Program Director of the Exercise Science program and Exercise Oncology certificate program at Wright State University. I’m also privileged to serve as the Founding Director and CEO of Maple Tree Cancer Alliance and am honored to be a Fellow of the American College of Sports Medicine (FACSM). My academic journey culminated with a Ph.D. from the University of Northern Colorado in Exercise Science, with specialized focus on Exercise Physiology and Cancer Rehabilitation.
My career has been dedicated to developing evidence-based exercise programming for cancer patients and survivors, with a primary focus on improving quality of life outcomes through precisely prescribed exercise interventions. Over the years, I’ve been fortunate to secure multiple grants and establish numerous clinical partnerships that have allowed us to expand access to cancer exercise programs not only across the United States but also in 23 countries worldwide.
As director of the Wright State University Cancer Resource Center, I work to advance the field of exercise oncology through innovative research and by creating interdisciplinary, experiential learning opportunities for students. This center serves as a hub for both research development and workforce training in this specialized field.
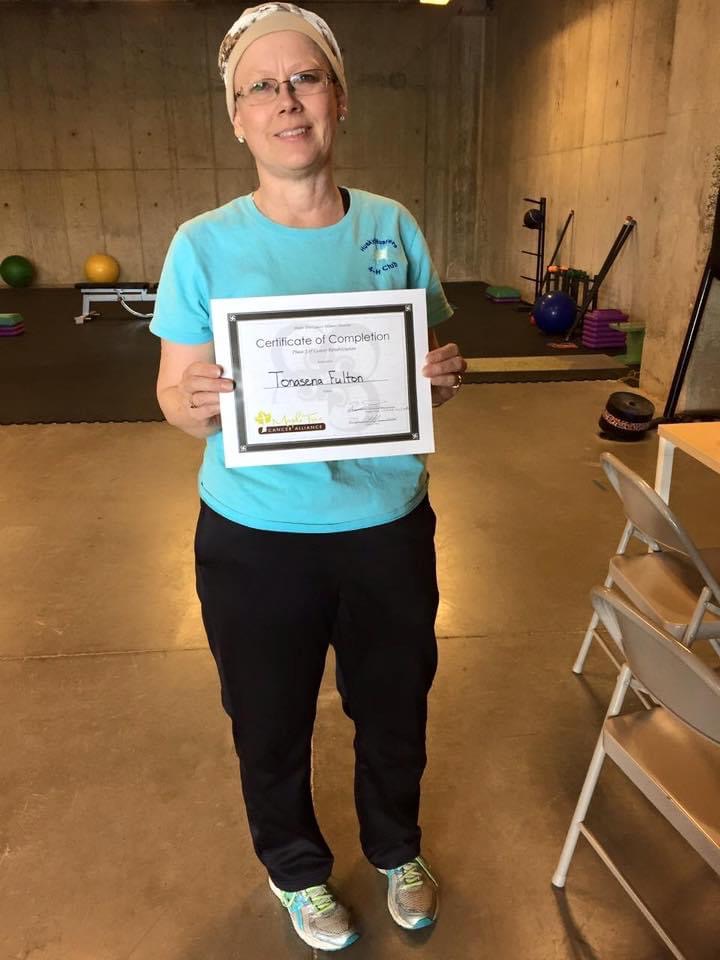
What truly distinguishes our work at Maple Tree Cancer Alliance is our successful implementation of exercise oncology programs within healthcare systems across multiple states. These programs have brought exercise-based rehabilitation services to thousands of cancer patients annually. Our approach centers on creating individualized exercise prescriptions that address the unique needs of cancer patients throughout every stage of their treatment journey.
Throughout my career, I’ve been particularly passionate about developing professional education programs for healthcare providers and exercise specialists in cancer rehabilitation. This effort has been instrumental in building a qualified workforce capable of delivering specialized care to this vulnerable population.
I believe what sets our approach apart is the seamless integration of rigorous academic research with practical clinical application. My work continues to focus on bridging the gap between research findings and their implementation in clinical settings, making exercise-based interventions more accessible and beneficial to cancer patients and survivors.
What I’m most proud of are the more than 200 student interns I’ve had the privilege of mentoring over the years. Watching these students grow into compassionate, skilled professionals who carry this important work forward has been among my greatest professional joys. These graduates are now working in cancer centers nationwide, expanding access to exercise oncology services and conducting important research that continues to advance our field.
For those considering our services at Maple Tree Cancer Alliance, I want them to know that movement truly is medicine—perhaps the most accessible and empowering medicine available during cancer treatment. Our programs meet patients exactly where they are, whether they were highly active before diagnosis or have never engaged in structured exercise. And for students interested in this field, we offer not just technical training but a philosophy of care that centers human dignity and resilience above all else.

Other than training/knowledge, what do you think is most helpful for succeeding in your field?
I’ve found that beyond formal education, several key qualities are essential for success in exercise oncology—with empathetic resilience topping the list.
Working with cancer patients means witnessing suffering regularly. You’ll guide people through perhaps the most difficult period of their lives, and some patients won’t survive despite your best efforts. This emotional reality requires a unique form of resilience that combines compassion with the ability to process grief without becoming overwhelmed.
What’s helped me develop this “grit” over the years:
Finding meaning in difficult moments. When a session is challenging or when a patient is struggling, I focus on the purpose behind our work. Exercise isn’t just about physical metrics—it’s about giving patients agency during a time when they feel their bodies have betrayed them.
Building a support community. I meet regularly with colleagues who understand the emotional weight of this work. Having safe spaces to process difficult experiences prevents compassion fatigue and isolation.
Celebrating small victories. In exercise oncology, success often looks different than in traditional fitness. A patient who can climb stairs again to tuck their child into bed represents a profound victory, even if their physiological markers haven’t dramatically improved.
Practicing self-care consistently. I’ve learned—sometimes the hard way—that I cannot effectively support others if I’m depleted. Regular physical activity, mindfulness practices, and maintaining boundaries between work and personal life have been essential.
Embracing a growth mindset. The field of exercise oncology is constantly evolving. Being comfortable with uncertainty and viewing challenges as opportunities for development rather than obstacles has been crucial.
The students who thrive in this field aren’t necessarily those with the highest academic credentials—they’re the ones who can hold space for a patient’s pain while simultaneously helping them build strength. They’re the ones who can adapt when a carefully planned exercise protocol needs to be modified because the patient is having a difficult day.
This kind of grit isn’t innate—it’s cultivated through practice, reflection, and a deep commitment to the people we serve. It’s developed by staying present during difficult conversations and by continuously asking yourself: “How can I better serve this person in front of me?”
How about pivoting – can you share the story of a time you’ve had to pivot?
When COVID-19 lockdowns were implemented five years ago, we faced what seemed like an insurmountable challenge at Maple Tree Cancer Alliance. Until that point, the concept of virtual exercise training for cancer patients was considered virtually impossible. The prevailing wisdom in our field held that the safety concerns and efficacy requirements for this vulnerable population demanded in-person supervision and monitoring.
Then suddenly, overnight, we had no choice. Our patients—many immunocompromised from treatment—couldn’t risk coming to facilities, yet they desperately needed to maintain their exercise regimens. What happened next demonstrated the remarkable resilience of both our team and our patients.
Within 48 hours of lockdown announcements, we mobilized every resource we had. Our staff worked through the weekend, rapidly developing protocols, testing video platforms, creating modified home-based exercise prescriptions, and personally calling every patient. By Monday morning, we had successfully transitioned 84% of our patient population to virtual exercise sessions—something previously thought unachievable in our field.
The response was immediate and powerful. One patient, who was undergoing aggressive chemotherapy for colorectal cancer, told us, “Your virtual sessions are the only reason I get off my couch each day.” Another, an elderly woman living alone during treatment, confided, “You’re the only human being I’ve spoken to today.” These weren’t just exercise sessions—they had become lifelines during an isolating and frightening time.
Recognizing the groundbreaking nature of this shift, we quickly designed and received IRB approval for a study to evaluate the safety, efficacy, and feasibility of virtual exercise training for cancer patients. The data we collected over those first 12 weeks was revelatory. Not only was virtual training safe and feasible, but the outcomes in terms of physical function, quality of life measures, and adherence were comparable to our in-person programs. By the end of those 12 weeks, we had successfully transitioned 93% of our patients to virtual training.
What began as an emergency response evolved into a transformative approach for our organization. Five years later, two-thirds of our program partnerships are now virtual or hybrid models. This shift has dramatically expanded our reach, allowing us to serve patients with transportation limitations, those in rural areas without specialized facilities, and to partner with hospital networks facing space constraints.
The pandemic forced us to challenge our assumptions about what was possible in exercise oncology. In doing so, we discovered that with proper protocols and training, virtual exercise programs could deliver the physical benefits our patients needed while also providing crucial social connection and emotional support during treatment.
This experience taught us that innovation often emerges from necessity, and that our capacity to adapt in service of our patients’ needs is far greater than we might have imagined. What seemed unthinkable five years ago is now a cornerstone of how we deliver care.
Contact Info:
- Website: https://www.mapletreecanceralliance.org
- Instagram: https://www.instagram.com/mapletreecanceralliance/?hl=en
- Facebook: https://www.facebook.com/mapletreecanceralliance
- Linkedin: https://www.linkedin.com/in/karen-wonders-78b53b65/
- Youtube: https://www.youtube.com/@mapletreeeducation77